Royal Borough of Windsor & Maidenhead: local authority assessment
Downloads
Overall summary
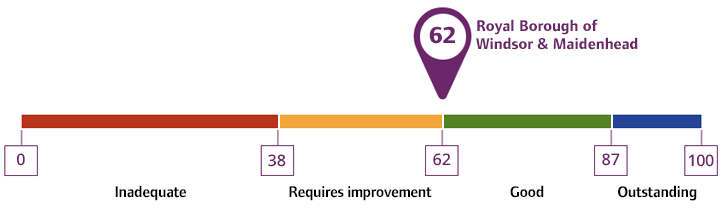
Local authority rating and score
Quality statement scores
Summary of people's experiences
People’s experiences of accessing adult social care in the Royal Borough of Windsor & Maidenhead were positive. National data supplied by the Adult Social Care Survey (ASCS) showed 68.83% of people were satisfied with their care and support. This was above the national average of 61.21%. Additional data provided by the local authority, but as yet unpublished, suggested further improvements had been made in this area in 2024. Staff conducted assessments which focused on people’s strengths and abilities. The feedback about the approach of staff and their competence was positive and this was reflected in compliments the local authority received. People received assessments and support from kind, dedicated and compassionate staff.
There was a front door team who had a good understanding of what was available to people with either eligible or non-eligible needs. We heard examples of how staff often worked with people at an early stage, before they developed eligible needs, to delay or avoid the need for more intrusive or restrictive interventions in the future. However, we heard feedback that young carers did not always receive a timely assessment and national data showed access to advocacy was limited. We also heard feedback that at times information was harder to find, particularly for older people who may face digital exclusion. These were areas where the local authority told us they had plans to improve. However, people who contacted the local authority often received a call or a home visit which reduced the impact of the gap in the information and advice offer.
The experiences of unpaid carers were mostly positive, but we did hear feedback that access to information and advice was not always consistent. Unpaid carers received their own assessment and we saw examples of care planning to meet their eligible needs. Unpaid carers spoke positively about the support available to them from the voluntary sector. Unpaid carers received an assessment in a timely way, but we did hear there was sometimes difficulty finding information related to the support available to them and some difficulty accessing assessments for young carers.
Staff worked closely with partners to meet people’s needs holistically. We received feedback about the voluntary services on offer to people and saw examples of positive joint working between health partners and the local authority to meet people’s needs. People received support from staff who worked closely with health partners, both at hospital discharge and at the front door team who received initial contact, to ensure the right support was available to people at the right time. Recent work to improve hospital discharge pathways through the ‘Home First’ model had brought about improvements to the time it took for people to be discharged from hospital; national data showed the reablement people received was achieving good outcomes and avoiding readmission to hospital.
Summary of strengths, areas for development and next steps
This assessment took place during a time of significant transformation. The local authority was bringing their Care Act 2014 functions in-house and many processes were currently being reviewed or were recently updated. As well as having recently introduced new teams, the local authority was about to introduce new IT systems and change their strengths-based model of assessment to a ‘Patchwork’ model which was intended to better enable staff to assess people’s needs around their strengths and assets. The relationships with health partners were also going through a period of transformation, with recent changes to the structures of the safeguarding partnership board, and the health and wellbeing board.
Despite significant transformation being underway, feedback from staff about the support they received during change was positive. Staff felt proud of the work the local authority did, and we heard multiple examples of positive, person-centred, practice being used to ensure people achieved good outcomes. Staff told us the transformation would improve the way they work, particularly around having better access to data, being more collaborative across teams and seeing improved consistency and oversight of performance. Staff were overcoming most of the challenges presented to them by the current systems, but recognised the transformation would lead to more sustainable processes and approaches.
The feedback from health partners was positive; despite change at the local authority and within the local health structures, we heard about positive working relationships focused on ensuring people were kept healthy and their care needs were met. The local authority and health partners had achieved particularly good outcomes on shared priorities around hospital discharge, but joint strategic work in areas such as public health and safeguarding were at an earlier stage in their development.
National data showed the experiences of people living in the Royal Borough of Windsor & Maidenhead were positive or in line with national trends. Data showed the local authority performed particularly well in how safe people felt, with 80.77% of people who used services stating they felt safe (ASCS) which was significantly above the national average of 69.69%. However, data also showed direct payment uptake was low, with Adult Social Care Outcomes Framework (ASCOF) showing 12.08% of people using direct payments to access services, significantly lower than the national average of 26.22%. Additional data provided by the local authority, but as yet unpublished, suggested improvements had been made in this area in 2024. Data provided by the Safeguarding Adults Collection (SAC) showed 58.33% of people lacking capacity were supported by an advocate, family, or friend. This was below the national average of 83.12%.
Leaders had a good understanding of where they needed to improve and where we identified shortfalls, there were already plans underway to address them. Actions taken recently were clearly tethered to the overarching transformation strategy, but some changes had yet to take place or to fully embed. Changes had already been made to improve approaches to safeguarding and update the information and advice offer. Changes to areas such as co-production and commissioning had started but were at an earlier stage, whilst new IT systems to bring about improvements in the use of data had yet to be implemented.
Data was used by the local authority to measure the impact of improvements and measure the impact on people’s experiences, but the use of data was limited by the current systems. We heard from staff and leaders that sometimes data was time consuming to collate and the ability to compare and interrogate data was limited. However, where data was available the local authority was able to use it to demonstrate the positive impact of recent changes. For example, the introduction of the new safeguarding hub had reduced waiting time for decisions about safeguarding concerns and staff described improved consistency in decision-making in this area.
Waiting times for Care Act 2014 assessments had also been reduced, but there was a wait of up to six months for occupational therapy assessments. Staff and leaders had a good understanding of risks within waiting lists, and we heard how initial triage led to interim care provision arrangements being put in place ahead of full assessments. Unpaid carers received timely assessments most of the time, but data showed there was a slightly longer wait time for young carers assessments. The local authority recognised their current systems made data difficult to collate which meant it wasn’t always easy to monitor waiting lists. However, the processes in place meant all cases were being regularly checked and risk assessed. This area of improvement was a strategic priority; the local authority’s plans to introduce new systems were driven by the need to improve their oversight of data.
There had been recent changes to public health, and we saw examples of improved use of data to understand the health needs of the population, with data being used to keep people healthy and anticipate future need. Data had been used to set some strategic priorities, particularly around commissioning and hospital discharge pathways. Health partners and staff described positive working relationships and joint working to achieve shared aims. We heard about a strong and thriving voluntary sector but did hear some feedback on how it could sometimes be difficult to contact the local authority or work with them strategically. The public health team were considering new ways of co-productive working in specific cases. For example, they were working with the Primary Care Networks to shape Tier 2 weight management services alongside the practices and their users.
Staff and leaders had a good understanding of diverse communities across the Borough, and they knew who their seldom heard groups were. We saw examples of particularly positive outcomes being achieved for some groups which had drawn interest from other local authorities, but strategic work to positively impact other groups had not yet shown its full value. Whilst some of the strategic work was at an early stage, we saw how creative approaches had been taken in setting up groups or undertaking work with individuals to meet their needs in a way which was considerate of their preferences and any protected characteristics. Whilst some work was achieving good outcomes, planned actions such as updating the autism strategy, or improving commissioning for people with a learning disability, had not yet been fully realised.
We heard positive feedback about leaders, and staff understood the strategic direction and vision of senior leaders. The local authority had an ambition to introduce a performance culture, and we saw examples of how understanding and reporting of performance had improved over the last year. The local authority had planned for the new IT systems with a view to improve their ability to collate and monitor data; this part of the transformation had not happened yet, so there were areas where access to data was limited, but interim arrangements reduced the impact on service and strategic planning.